Tailored solutions to suit client needs
We work with insurers, brokers, MGAs, corporates and public entities to deliver great customer service and improved underwriting performance, through efficient management of the claims process.
Services
Our people

Allison Carr
Chief Executive Officer (UK&I)

Gary Fitzpatrick
Chief Strategy & Development Officer (UK&I)

James McEwen
Chief Client Officer (UK&I)

Jo Wells
Chief Finance Officer (UK&I)

John Salt
Chief Information Officer (UK&I)

Laura Warwick
Chief Operating Officer, Complex & Specialty (UK&I)

Liz Meagher
Chief HR Officer (UK&I)

Richard Greer
Chief Operating Officer, Core & Volume (UK&I)

Pamela Davies
Market Director – Personal Lines (UK&I)

Andrew Evans
Market Director – Broking & Major Risks (UK&I)

Samantha Ramen
Market Director – Commercial Lines (UK&I)

Connie Cobb
Market Director – Specialty Lines (UK&I)

Conor Kennedy
Head of Ireland Claims

Enrico De Micco
Director of Claims - Italy
Working With Us
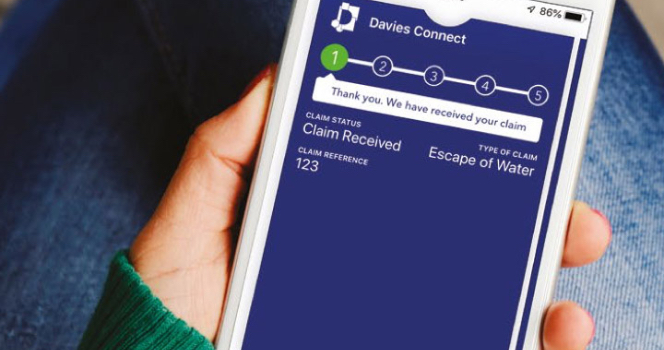
We enhance our service with technology to deliver cost and time savings to our customers.
How we've helped our clients
Latest news & insights
Featured Articles
-
Trouble with tenants: Victory for our client in missing handrail case
-
Our thorough investigation saved legal costs in discontinued slip and fall claim
-
Article
Q&A: Davies on the claims handling applications of AI
This article was first published by Insurance Times. Jon Glover, director…
-
Article
Responsible Business is Good Business: How to Implement Responsible Business Initiatives
With sustainability and ethical conduct becoming increasingly important to the modern-day…